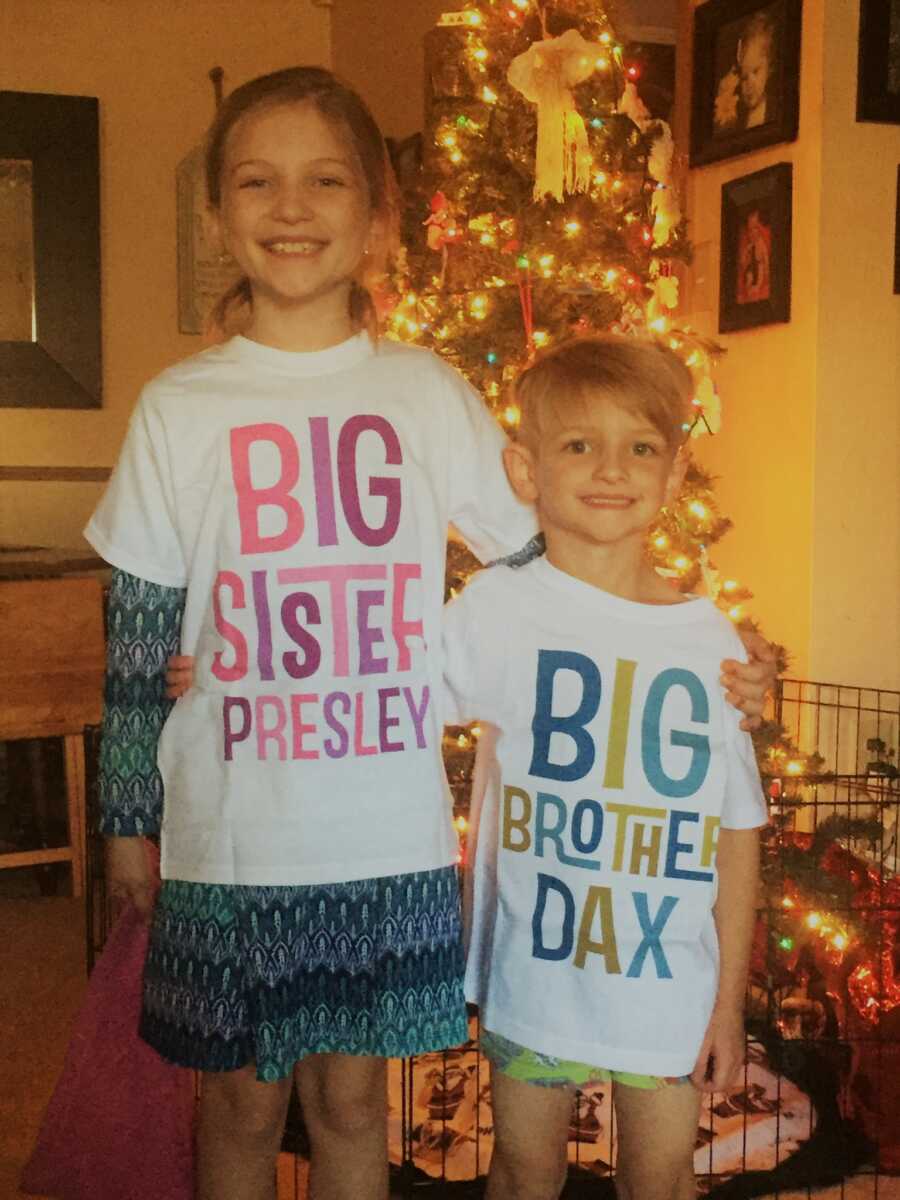
“I always envisioned myself with 4 kids. Not sure why exactly? I just always have. In December of 2006, 13 months after we got married, we lost our first baby. It was devastating! Months of negative tests and heartbreak led to our rainbow baby. Our daughter, Presley, was born in 2008, and our son, Dax, followed in 2010. As the years passed, I still yearned for that 4th baby. Like most husbands,
Jeff was worried about the financial aspect of it, which is why years passed before we tried again. When we found out we were expecting in late 2016, EVERYONE was excited! Since we had a girl and a boy, we decided this time, we were going to wait until the birthday to find out the gender. The suspense made this last pregnancy so much fun! Other than morning sickness the entire pregnancy,
our baby looked great and we had no problems. The last few weeks of the pregnancy I did start to notice less movement and even went to labor and delivery a few times. (Having lost one baby, I was always afraid it would happen again.) I would get hooked up to Doppler and hear the heartbeat and was sent on my way. At one of my last weekly checks, my doctor even sent me for a doppler due to a lack of fetal movement. Again, doppler, heartbeat, home.
August 22, 2017, the big day. We walked into the hospital that day thinking our big surprise was going to be the gender reveal; if only that were the case. Prior to going into the O.R., I filled out paperwork for a pilot program using my placenta for skin grafts for burn victims. What a privilege! Going into the O.R. we were riding a high! It was baby time.

As soon as the baby came out, Jeff and I instantly knew something was wrong. There wasn’t any crying. We heard a tiny squeak and nothing else. Dr. M said, ‘It’s a girl’ and quickly showed her to me and handed her off to the nurses in the delivery room. Something was wrong. I told Jeff, ‘Don’t leave her. Please don’t leave her.’ The nurses continued bagging her with oxygen.
‘What’s wrong?’ I kept asking. Her lungs were sticky, and she needed to be taken to the NICU, they said. Soon after, NICU doctors informed us that she was gravely ill and that they had done everything they could to help her. Dallas Jane Parker was born full-term and with a lot of shocks. She had a collapsed lung, a prematurely collapsed lung, an elevated right diaphragm, and significant pulmonary hypertension when she was born. She was intubated, given a chest tube, and placed on an oscillating ventilator right away.

Doctors told us our daughter wasn’t going to make it. I can’t explain it, but I was mad! I didn’t cry, I got angry. I said, ‘You are known for your NICU. Women come here to have their babies specifically because of your NICU. Don’t tell me you’ve done all you can do. You better figure it out!’ We had them call in a sweet little clergyman to baptize her in the NICU, in case what they were saying was true. The doctor came back and said her only chance of survival, as slim as it would be, would be to get placed on ECMO (Heart and Lung Bypass).
A machine had just opened up at another hospital. We were informed of the risks involved in moving her in her unstable condition, but if we stayed where we were, she was going to die. If we moved her, she might die before she arrived at the other hospital, but she might hang on. We had to go for it. Jeff left with Dallas and I was left in shock. I soon found out, my placenta would not be eligible for use either. About a 1/4 of it had calcified with Dallas in it.

When Jeff arrived in the ICU at Medical City Children’s Hospital Dallas, he was congratulated. She’d made it alive, but was in for the fight for her life, with a team of doctors and nurses who NEVER gave up on her. Dallas survived being placed on ECMO, another HUGE feat. I couldn’t stand it. I was a half-hour away from my baby who is standing on death’s doorstep.
I had no choice but to accompany her. Only a few times had I seen her face and touched her skin. If my kid were to leave this earth, she would do so with her mother telling her how much she is loved. Kim, a great friend, arrived in my room with a cart and began filling her car. My OB recognized my need to be with my kid, so I departed roughly 24 hours following the C-Section. I was disappointed that Presley and Dax did not get to meet their sister for the first time, but I am grateful that the physicians were able to make it happen despite the gravity of the situation.

Seeing her for the first time, and the cannulas coming out of her neck, the lines in her groin, was devastating, but you have to put that emotion away and keep moving forward. On day 6 1/2, we were informed her pulmonary hypertension had resolved, and we could trial coming off ECMO the following week. We were ecstatic!
The next morning we walked into controlled chaos. We were told Dallas was bleeding to death internally (lung and heart) and had a blood clot in the cannula going into her body. She just had minutes to live. We were told, ‘Say what you need to say because we have to get started.’ How do you say goodbye like that? We told Dallas how much we loved her and begged her to be strong. We begged her to come back to us. I remember telling one of the ECMO specialists,

‘Do your best.’ Isn’t that weird? My daughter’s life was hanging in the balance and that’s what came out. ‘Do your best.’ It was also time for me to pump. Both of us hysterically crying, I pumped milk I didn’t know if my baby would be alive to eat. Our baby is a warrior! She made it through all 3 procedures when they didn’t know if she would make it through one.
One week later, we were dropping the kids off at school and the hospital called. Dallas coded, requiring compressions. Rush hour traffic took an hour and a half to get there. We almost lost her again. The trauma of CPR caused her to develop systemic capillary leak syndrome. She doubled her weight in fluids overnight. This would be the next battle for her life. She had to be placed in a medically induced coma, as she was so swollen her eyes had swollen shut. Dallas looked like she had been in a nasty fight, cauliflower ears and all. Her skin was splitting open and bleeding, and she was weeping fluids from everywhere.
At 23 days old, Dallas was finally stable enough for us to hold her for the first time. It took 5 people over 30 minutes to make that happen, (3 ICU nurses and 2 RT’s) and it was totally worth the wait! From there, Dallas had recurrent chylothorax (her body was leaking fats and proteins into her chest cavity), requiring three additional chest tubes, a tracheostomy, and a G-tube. After nearly 6 months in the hospital, she came home. We get asked all the time if traching our baby was a hard decision.

The answer is no. Was it scary? ABSOLUTELY! Traching Dallas Jane was the single best decision we have made in her life. Being trached has allowed her mobility, the ability to vocalize, and in her case, speak in full sentences. Being trached gives her freedom. It gives her a chance at a ‘normal’ life. One day, when we have her seizures fully controlled, we will decannulate (kiss that trach goodbye). It is a day we dream about.
Dallas Jane just turned 4 in August. She has literally spent half of her 4 years inpatient. We have been told more times than we can count, ‘She isn’t going to make it,’ ‘She’s just too sick,’ ‘Her body is tiring out. You better call Jeff to get up here.’ Her list of conditions has continued to grow. At times it’s overwhelming. She has chronic respiratory failure (which she will outgrow), exotropia in both eyes, hypoplastic enamel on her teeth, mobility issues (she started walking earlier this year, still a little wobbly), poor immune system, Hashimoto’s Encephalitis, Hashimoto’s Thyroiditis, Graves disease, complete thyroidectomy, mediport, Epilepsy, PTSD, anxiety, panic disorder, G/J tube, hypertension, and dysautonomia, to name a few.
We have done genetic testing (including whole-exome sequencing) and she hasn’t been linked to anything. We call her the unicorn. She collects rare diagnoses and stumps doctors everywhere. We have asked for several second opinions at places like Mayo and Boston Children’s and have discussed the Undiagnosed Network with one of her geneticists.

Due to all of Dallas’ conditions, her doctors have told us it isn’t safe for us to travel alone. She needs medical transport. We were just in the hospital for 104 days, but COVID shot down our chance for a transfer and a second opinion. Covid has made this life incredibly difficult. In 2020, Dallas spent 200 days inpatient, and in 2021, 145 days inpatient. We had some scary close calls and the ‘one parent in and one parent out’ rule made having a child close to death unbearable.
At one point, Dallas was going downhill fast. I called Jeff to come immediately. They let us both in and gave us the opportunity to stay with her during a procedure as they were sure, if it didn’t work, she would pass. She pulled through. They gave us 5 minutes to be together with her, and then I was told I had to leave. 5 minutes. My daughter was almost no longer living 5 minutes prior and I am supposed to be okay leaving her. It was truly one of the hardest things we have had to go through yet.
Dallas’ epilepsy has been incredibly difficult. She has had seizures that last anywhere from 30 seconds to 90 minutes. Dallas often stops breathing as soon as the seizure starts. Quite often, it takes bagging (CPR breathing through her trach) with 15 liters of oxygen to bring her color from blue to a pretty pink again. Her oxygen saturation has dropped as low as 2% during a seizure. NOTHING on this earth prepares you to see your child any shade of blue or grey. It’s absolutely terrifying.
She has just about every kind of seizure you can have, and none of her lobes discriminate. Her epileptologist has warned us she is at a very high risk for SUDEP (sudden unexpected death by epilepsy). Dallas is approved for 24/7 in-home nursing, but due to a lack of nurses and an overwhelming lack of skilled/trained nurses, we’ve gone without. We have trained our older children in all of her cares, as it often takes more than one set of hands in emergencies.
They have breathed for Dallas when she isn’t able to do so, while we are pulling emergency seizure meds. Our older two, have literally breathed life back into their sister. They have had to help resuscitate her and then walk out the door for school. Forced into growing up too fast. Innocence lost. They have seen and done things countless times that most people will never do once in their lifetime. They are true rock stars and absolute heroes in all of this.
They are the most compassionate, empathetic, kind kids, who have learned life looks different for different people, and they find beauty in that. They’ve learned people aren’t disabled, they are abled differently. We are so proud of them. One of the hardest parts of this journey, besides seeing Dallas in pain or distress, lack of answers and/or action, is the complete isolation that comes with it. In order to bring her home, one of us had to quit our jobs.

Jeff is the breadwinner so it was a no-brainer; I would stay home. (We were NOT ready to take that financial hit by the way.) I had my own identity. Teacher, employee, coworker, friend, wife, mom, etc. I left like I lost my identity altogether. I am now, nurse, PT, OT, speech, taxi, scheduler, advocate, social worker, supply chain, nutrition, behavior therapy, pharmacist, wife, soccer mom, choir mom, etc. My identity revolves around Dallas mostly.
When Dallas was born, the support was so thick you could feel it. Over time, your friends stop inviting you to do things, and eventually stop calling and texting altogether. I get it right? They don’t understand our life now and probably don’t know what to say; so they say nothing. To be honest, my social life is social media. With no nurses, there are no girls’ days or even date nights with Jeff. I don’t have an adult conversation unless she has doctor appointments or gets admitted. Then I get so excited I’m sure I talk their ears off.
I feel like 4+ years in, we’ve become so isolated I feel socially awkward when I do get out. I don’t have anything to talk about but Dallas. With Dallas being immunocompromised, taking her out in public is a risky move. We’ve never been out to eat as a family of five. Dallas has never been in a store of any kind, or anyone’s house but ours.
She is either at home, the hospital, or the doctor’s office. We are ready to start getting her out, and she is getting stronger, but a common cold could still kill her, and that scares the hell out of us! We have ‘met’ and rely on the support of other parents in situations similar to ours. The trach, tube feeding, Epilepsy, and Tiny SuperHero groups have led us to some incredible people who have been an amazing outlet and source of comfort. We are grateful for them.
Our lives are drastically different than before she was born. It is very easy to see all the things we have lost, and all the things we can no longer do. It’s also easy to see we are witnessing a miracle in the flesh. Dallas Jane is the feistiest little girl with an incredible fight within her. We will ALWAYS advocate for her. We will NEVER give up on her.
Dallas is the perfect, final piece to the Parker family puzzle. The thing that makes us ‘The Parker 5.’ Dallas breaks every barrier set in front of her and defies the odds time and time again. Dallas Jane Parker arrived on August 22, 2017, full-term and full of surprises. She continues to live by that motto.”
